Inflammatory biomarkers across a range of human diseases
- Clinical research , Inflammation , Protein biomarkers
- Read time: 8 minutes
Olink panels targeting inflammation-related proteins suggest new pathophysiological mechanisms across diverse disease areas. This brief review shows how cytokines, chemokines and other immune- and inflammatory proteins are integrally involved with infectious disease (COVID-19 response), neurology (traumatic brain injury), digestive disorders (ulcerative colitis) and skin disease (atopic dermatitis).
Inflammation can be chronic
Inflammation is characterized by the activation of immune and non-immune cells to protect the host organism against pathogens and related toxins by eliminating these infections, establishing immune memory and promoting tissue repair and recovery. Recent research has uncovered differences between a normal acute inflammatory responses (where inflammatory activity is up-regulated for a short period of time) and low-grade, non-resolving “systemic chronic inflammation” that is characterized by activation of immune components but is persistent, breaking down immune tolerance and leading to major changes across tissues and organs.1
To study a complex and pervasive inflammation-related pathogenesis, Olink Proteomics offers the broadest and most comprehensive set of multiplexed inflammation biomarker assays on the market. These sensitive biomarker panels scale from the Olink® Target 48 Cytokine panel (simultaneous analysis of 26 cytokines, 12 chemokines and other immune-related biomarkers totaling 45 protein targets), through the Olink® Target 96 Inflammation panel (simultaneous analysis of 92 protein biomarkers), up to the Olink® Explore 384 Inflammation I and Olink® Explore 384 Inflammation II panels, each with approximately 370 inflammatory or inflammation-related biomarkers each. Here we highlight four diverse disease areas where Olink panels revealed a central role for inflammation-related proteins: severe COVID-19, traumatic brain injury, ulcerative colitis and atopic dermatitis.
Inflammation markers involved in severe COVID-19 and cytokine release storms
A recent meta-analysis across five independent COVID-19 studies analyzed 253 unique proteins (contained in the Olink® Target Inflammation, Cardiovascular II and Cardiovascular III panels) that were common to all.2 The number of cases, and the fourteen proteins differentially expressed, are shown in Figure 1. Thirteen of the proteins were overexpressed in COVID-19 patients across all five studies (CCL7, CXCL10, CCL8, LGALS9, CXCL11, IL1RN, CCL2, CD274, IL6, IL18, MERTK, IFNg, and IL18R1) with only one (CCL16) that was higher in healthy controls. Figure 2 shows the heatmap with the five studies listed on x-axis and the fourteen differentially expressed proteins on the y-axis.

Figure 1: Five cohorts used in the COVID-19 meta-analysis from Suhre et al.1
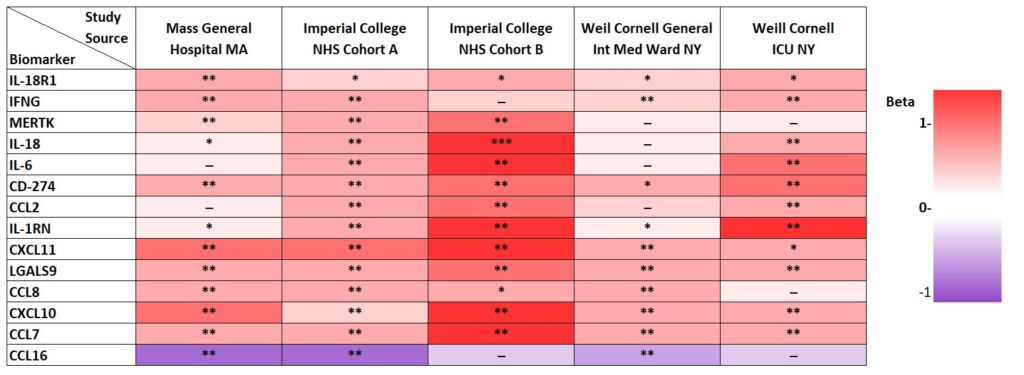
Figure 2: Heatmap analysis of 13 statistically increased and decreased levels of protein biomarkers in COVID-19 patients patients out of a total of 253 measured across studies. Significance “**” (p<0.05/253/5 = 4×10-5, Bonferroni level), “*” (P<0.05/115 = 0.00043, replication level), “–” (p<0.05, nominal significance). Adapted from Suhre et al. Figure 5a.2
In this meta-analysis they noted that several immune pathways were activated, including viral protein interaction with cytokine and cytokine receptors, and the COVID-19 adverse outcome pathway, with particular emphasis on CCL2, CSCL10 and IL6. Another interesting point to make is that in spite of the diversity of settings, sample type (serum or plasma) and sample handling from three different clinical settings, all of the data could be combined and statistically-significant findings be derived.
If you are interested in seeing a webinar on how high-throughput proteomics is a keystone in multiomics approaches to COVID-19 research, you can access it here.
Severe traumatic brain injury and markers of mortality
Traumatic brain injury (TBI) is a major cause of death and disability and is diagnosed clinically on a scale from mild to severe. In a study that measured 1,161 plasma proteins from the Olink® Target 96 panels in patients with severe TBI and known clinical outcomes, the top 15 differentially expressed proteins in the patients with sTBI mainly involved vascular pathology, immunity/inflammation, and cell survival.[3]
The researchers identified two protein biomarker pairs (vWF/WIF-1 or vWF/CSF-1) as potential disease severity or outcome biomarkers, as they were able to predict ICU mortality with 100% accuracy (Figure 3).
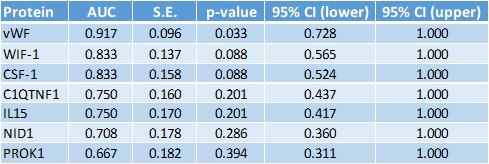
Figure 3: Receiver operating character curve analysis with TBI mortality as outcome, adapted from Fraser et al.3
Inflammation markers and early immune activation in ulcerative colitis
In ulcerative colitis (UC), immune dysregulation is dependent upon both genetic and environmental factors. Shifts in the microbiome and subclinical inflammation are defined by NFκB activity, and early detection markers are needed.
Plasma samples from patients up to 15 years pre-diagnosis (n=72) were tested along with patients with UC (n=101) with the Olink® Target 96 Inflammation panel, identifying a six-protein signature with excellent discrimination (AUC = 0.92).4 These pro-inflammatory and tissue-repair pathway proteins can detect UC several years before conventional diagnosis.
Inflammatory protein responses to a JAKi/SYKi for atopic dermatitis
In an example from drug development, a new dual inhibitor compound called ASN002 (from Asana Biosciences) for the condition atopic dermatitis was evaluated for efficacy, safety, pharmacokinetics, dosage and effects on systemic biomarkers.5
In a clinical trial (NCT03139981), a total of 36 patients were randomized and given three different doses or placebo, and patient samples were analyzed with four Olink® Target 96 panels (~360 total proteins). ASN002 significantly downregulated several serum biomarkers involved in Th1, Th2, and Th17/Th22 immunity, showing strong efficacy with not only rapid onset of action but also improvements in overall systemic inflammation.
In addition, their dosage trial indicated that a lower dose could be selected for optimal effect and decreased risk for adverse events.
Information about our Olink Target 96 Inflammation panels can be accessed here.
References
- Fullerton JN and Gilroy DW. Resolution of inflammation: a new therapeutic frontier. Nat Rev Drug Discov. (2016) 15(8):551-567. doi:10.1038/nrd.2016.39
- Suhre K and Schmidt F et al. Identification of Robust Protein Associations With COVID-19 Disease Based on Five Clinical Studies. Front Immunol. 2022 12:781100. doi:10.3389/fimmu.2021.781100
- Fraser DD and Prassas I et al. Novel severe traumatic brain injury blood outcome biomarkers identified with proximity extension assay. Clin Chem Lab Med. 2021 59(10):1662-1669. doi:10.1515/cclm-2021-0103
- Bergemalm D and Halfvarson J et al. Systemic Inflammation in Preclinical Ulcerative Colitis. Gastroenterology. 2021 161(5):1526-1539.e9. doi:10.1053/j.gastro.2021.07.026
- Bissonnette R and Guttman-Yassky E et al. The oral Janus kinase/spleen tyrosine kinase inhibitor ASN002 demonstrates efficacy and improves associated systemic inflammation in patients with moderate-to-severe atopic dermatitis: results from a randomized double-blind placebo-controlled study. Br J Dermatol. 2019; 181(4):733-742. doi:10.1111/bjd.17932
Upgrade your inflammation research
Find out more about why protein biomarkers can transform your inflammation research.
How the proteome behaves in healthy individuals
Clinical research, Multiomics
To achieve the goal of precision medicine, not only do different molecular profiles need to be understood in disease populations, but they must also be understood in the context of healthy populations.
Key proteomics publications from 2020
Proteomics
Welcome to the first post of the all-new weekly Olink to Science! Our customer survey revealed that you would like to know more about the many publications, research, and other science happening at Olink, therefore this blog aims to do just that: keep you informed on the exciting science taking place with our technology.
Protein biomarkers are crucial in early detection of cancer
Clinical research, Oncology, Protein biomarkers
A central premise of precision medicine is to identify biomarkers indicative of disease transitions early on. This is especially important in cancer where early treatment intervention could increase a patient’s chance of survival and reduce the probability of cancer recurrence.
Using PEA and RNA-Seq to study disease pathology
Clinical research, Proteomics
The following study illustrates how transcriptomics and proteomics complement one another to clarify the pathology of a complex, and little understood disease. Atopic dermatitis (AD) is the most common chronic skin condition affecting up to 20% of children and 7-10% of adults, depending on the population.
Olink protein biomarker panel indicates fermented foods fight inflammation
Inflammation, Proteomics
Could food be used to fight chronic disease?
Study identifies proteins involved in immunotherapy response
Oncology, Proteomics
'Ultimately, it is all about understanding and treating patients better in the future.'
Proteins diagnostic of lung cancer up to 5 years before disease onset
Oncology
An earlier Olink to Science blog post covered some amazing research that found that certain blood protein biomarkers have the potential to predict cancer up to 3 years before diagnosis. This may also be the case for lung cancer, as detailed in a recent study by Dagnino and her colleagues, where elevated levels of CDCP1 were detected in participants of a cohort who later developed the disease.
Utilizing proteogenomics technology for novel drug target discovery
Drug discovery & development
High-throughput multiplexed proteomic technology is leading the way to the latest developments in pre-clinical disease analysis in drug discovery. The pharmaceutical industry is now increasing its efforts in the discovery of novel drug targets by using protein quantitative trait loci (pQTLs), which allows for a more confident inference of disease causality and associated protein regulation.
Developing a high-performance biomarker panel for Alzheimer’s disease
Clinical research, Neurology, Protein biomarkers
A simple search of the term ‘scourge of Alzheimer’s Disease’ brings up over half a million website hits. A major disease, about 15% of us that reach the age of 67 to 74, and 44% of those 75 to 84 will develop AD.
How proteomics helped diabetic kidney disease research advance
Clinical research, Proteomics
Dr. Krolewski and his team at the Harvard Medical School found 56 proteins to be significant in diabetic kidney disease patients. Potentially, these could serve as prognostic biomarkers for disease progression and treatment response. This is how adding proteomics to the methodologies elevated their research.









